Safety Rate
Safety Rate
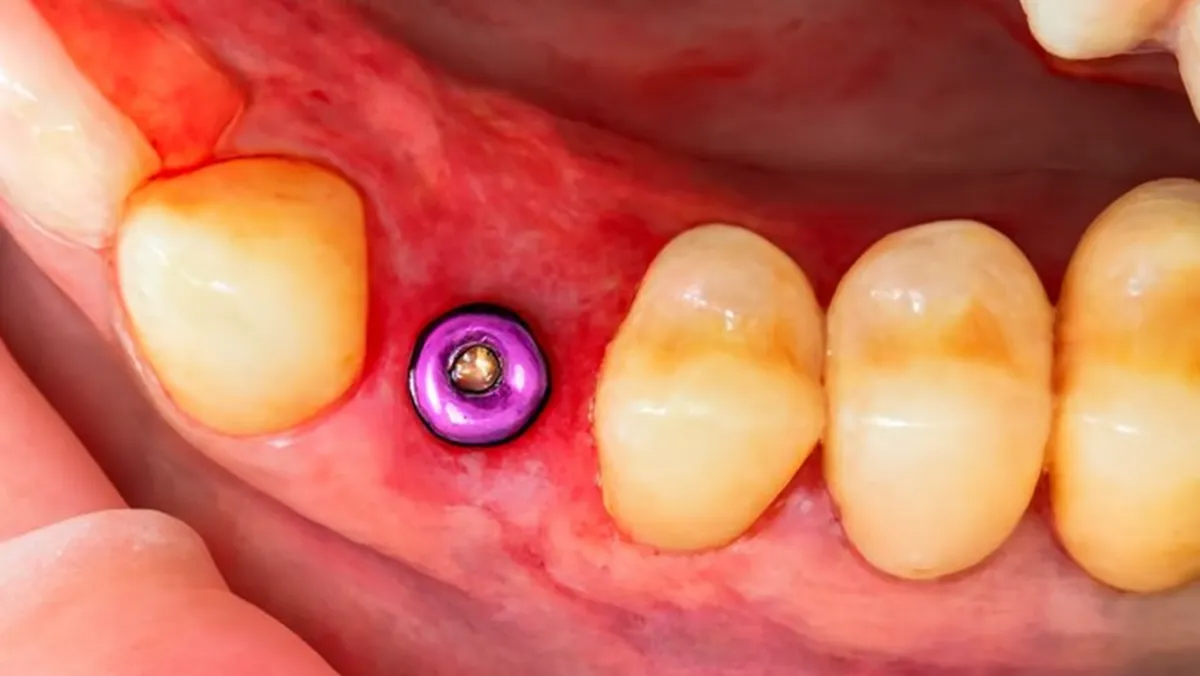
Dental implants are one of the most successful treatment options in modern dentistry, with survival rates typically above 95%. However, in some cases, implants may fail to integrate properly or develop complications over time. Failed implant management refers to the diagnosis, intervention, and treatment of these cases to restore oral health, preserve bone, and re-establish function. Implant failure can occur either early—when the implant does not fuse with the bone—or late, after years of function due to infection, overload, or prosthetic issues. Recognizing the signs of implant failure and intervening promptly is critical for minimizing damage and preserving future treatment options. Through careful evaluation, advanced imaging, and targeted treatment strategies, dentists can either salvage the implant, replace it, or redesign the treatment plan. Failed implant management is not only about addressing complications but also about restoring patient confidence, comfort, and long-term stability.
Implant failure occurs when a dental implant does not achieve or maintain stable integration with the surrounding bone. This may happen shortly after placement or years later due to biological or mechanical causes.
Understanding the reasons for failure helps clinicians design appropriate management strategies.
Recognizing symptoms early allows intervention before significant bone damage occurs.
Certain conditions and habits increase the likelihood of implant complications.
Accurate diagnosis is essential for deciding between salvage or replacement.
Treatment depends on the cause, severity, and stage of failure.
In some cases, implants can be preserved with corrective measures.
If the implant cannot be salvaged, removal may be the only option.
Post-extraction care focuses on preparing the site for future rehabilitation.
Prevention is the cornerstone of successful implant rehabilitation.
With proper management, re-treatment of failed implants can be highly successful.
Beyond clinical challenges, implant failure can affect patient confidence.
Failed implant management is a critical part of modern implant dentistry, ensuring that complications are addressed with professionalism and precision. While implant failure is rare, its impact on patients can be significant if not properly treated. Through early diagnosis, accurate evaluation, and tailored intervention, dentists can either salvage implants or plan for successful replacements. Preventive strategies, such as patient education, regular maintenance, and risk factor management, play an equally important role in long-term success. With advancements in imaging, surface decontamination techniques, and regenerative procedures, the chances of re-establishing a stable, functional, and aesthetic outcome are higher than ever. For patients, managing implant failure is not the end of their implant journey but rather an opportunity to achieve stronger, healthier, and more predictable results with the right treatment plan. Effective failed implant management restores not only oral function but also confidence and peace of mind.
Yes, in many cases a failed implant can be salvaged through non-surgical or surgical intervention. Early failures due to lack of osseointegration may require removal and replacement, while late failures from infection or overload can sometimes be managed with decontamination and bone regeneration. The success of fixing a failed implant depends on timely diagnosis, the extent of bone loss, and patient health factors. With appropriate intervention, patients often regain stability and enjoy long-term functional implants.
Common signs of implant failure include persistent pain, mobility of the implant, gum swelling, pus discharge, or visible bone loss on X-rays. Patients may also experience difficulty chewing or loosening of the attached crown or bridge. Early detection during follow-up appointments helps prevent severe complications. Dentists typically use clinical tests and radiographic imaging to confirm whether the implant has failed. Regular monitoring and good oral hygiene are essential for identifying issues early and ensuring long-term implant success.
The timing of replacement depends on the condition of the bone and surrounding tissues. If minimal damage has occurred, immediate replacement may be possible. However, in cases of infection or significant bone loss, implant removal is followed by bone grafting and a healing period of three to six months before re-placement. Careful assessment ensures the new implant has a solid foundation for long-term success. Following a tailored treatment plan significantly improves outcomes after implant failure.
Meet our experienced team of anaesthesiologists dedicated to your safety and comfort
Our experienced anaesthesiologists are here to ensure your safety and comfort